Value-based Reporting begins with Patient Input. Are you collecting Patient Reported Outcomes?
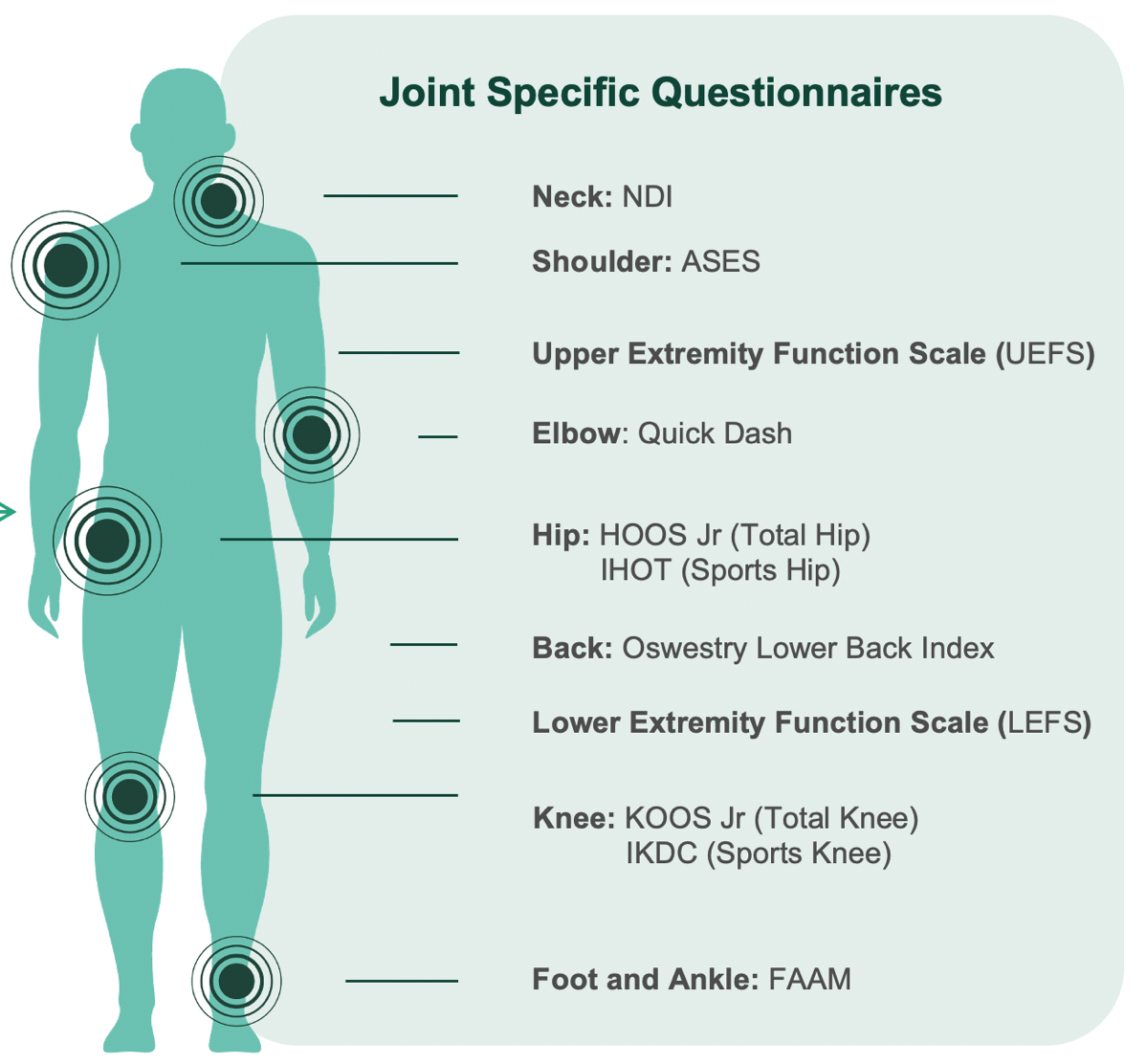
Sharecare is the leading digital health company, linking millions of people across the healthcare ecosystem. Through our unique OrthoQCDR collaboration, we have enabled the seamless collection of validated orthopaedic patient reported outcome questionnaires using Sharecare technology. By linking this information to your EMR system, we drive value to the entire practice by enabling treatment decision assistance and clinical results analysis in a variety of custom dashboards.
Collect the outcome information you need from the patient's mobile device before they arrive:
Drive value through the organization via custom dashboards that provide up-to-the-minute results of quality measures, patient input, record completion and provider results: